The cornea is one of the most underrated structures in the eye. Due to its transparency, many may not be aware of its existence or the crucial role it plays. The cornea is the transparent, dome-shaped window at the eye's front. It contributes to almost two-thirds of the eye's total refractive power, focusing light onto the retina in conjunction with the crystalline lens.
The cornea consists of five layers: the surface epithelium, Bowman’s layer, stroma, Descemet’s membrane, and the inner endothelium layer. The inner endothelium layer plays a crucial role in maintaining corneal clarity and hydration. The average corneal endothelial cell density (ECD) is highest at birth ranging between 4000 and 5000 (cells/mm²) and decreases at an average rate of approximately 0.6% per year in normal corneas throughout adult life.
Cataract surgery is one of the most common and safest single surgical procedures performed in the developed world, with approximately 10 million cataract surgeries done each year worldwide. However, it remains the leading cause of blindness in the developing world due to increased longevity and population growth.

“As the surgical armamentarium becomes more advanced and superior, the quality of outcomes and safety has substantially improved. Despite this, unforeseen complications may occur, potentially leading to unfavorable vision. One such complication is corneal decompensation, also known as pseudophakic bullous keratopathy (PBK) (Figure 1). Bullous keratopathy can occur in 1% to 2% of patients undergoing cataract surgery, which represents a small number compared to the approximately 10 million cataract surgeries performed each year worldwide,” said Dr. Lai Yin Peng, MBBS, MOphthal, CCFT Cornea, Cornea surgeon and consultant Ophthalmologist, KPJ Centre For Sight, Bandar Kinrara and PJ.
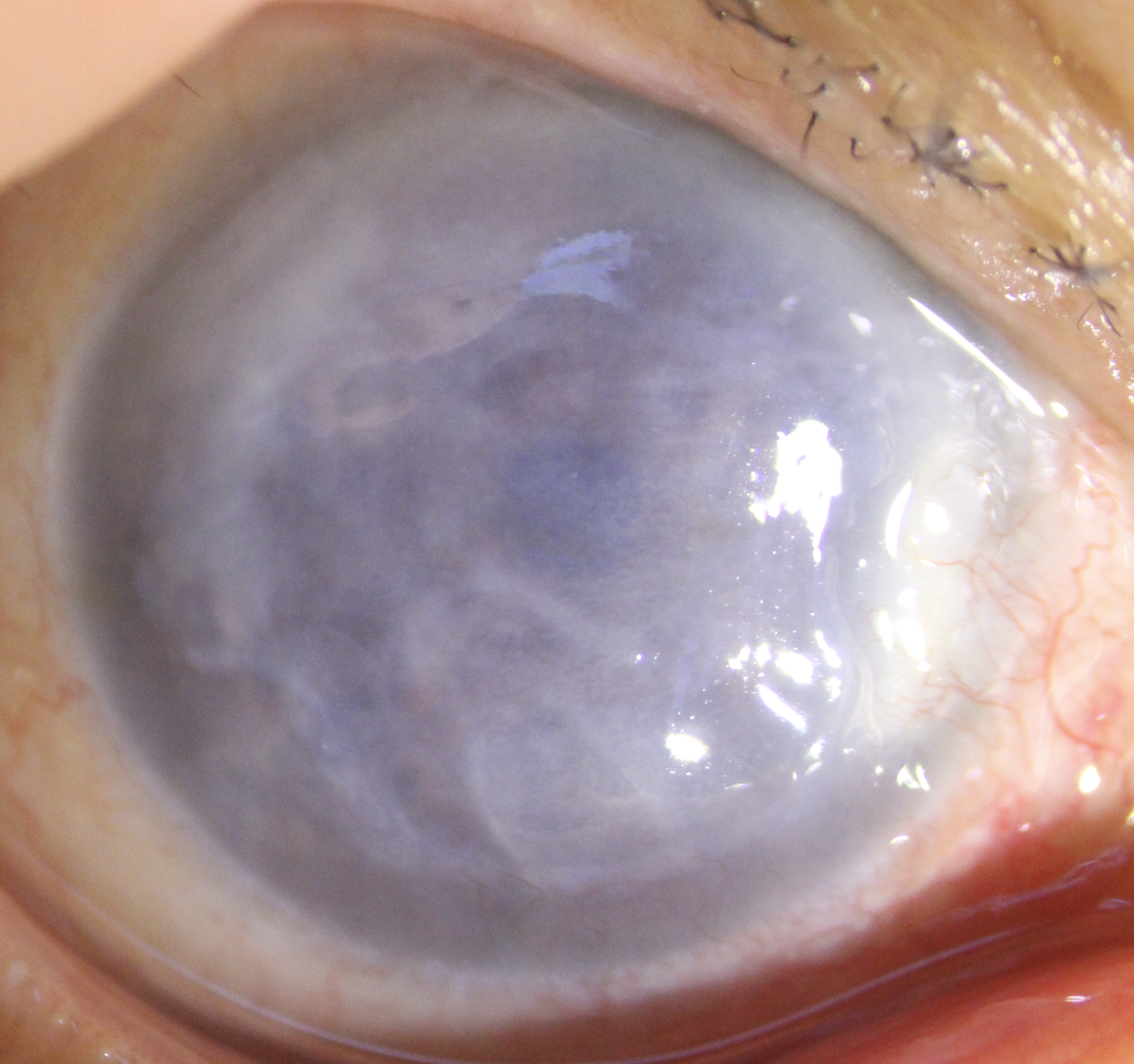
Bullous keratopathy is a condition where the cornea becomes swollen or edematous as the endothelial layer begins to lose its function in maintaining corneal transparency. These cells cannot regenerate themselves under normal conditions; thus, a significant loss in the number of cells leads to the onset of bullous keratopathy. The irreversible corneal edema or swelling starts with endothelial damage, followed by gradual stromal and epithelial edema. The formation of bullae or blister-like lesions occurs when the epithelium becomes swollen.
Any disease or external cause that disrupts the normal equilibrium and functioning of the endothelium can lead to bullous keratopathy. Eyes at higher risk of developing bullous keratopathy after cataract surgery include those with a pre-existing low endothelial cell count, especially in patients with Fuchs’ endothelial dystrophy, older individuals, those with a history of previous or multiple intraocular surgeries, previous ocular trauma, glaucoma, complicated cataract surgery (Figure 2), and systemic conditions such as diabetes and chronic obstructive pulmonary disease.
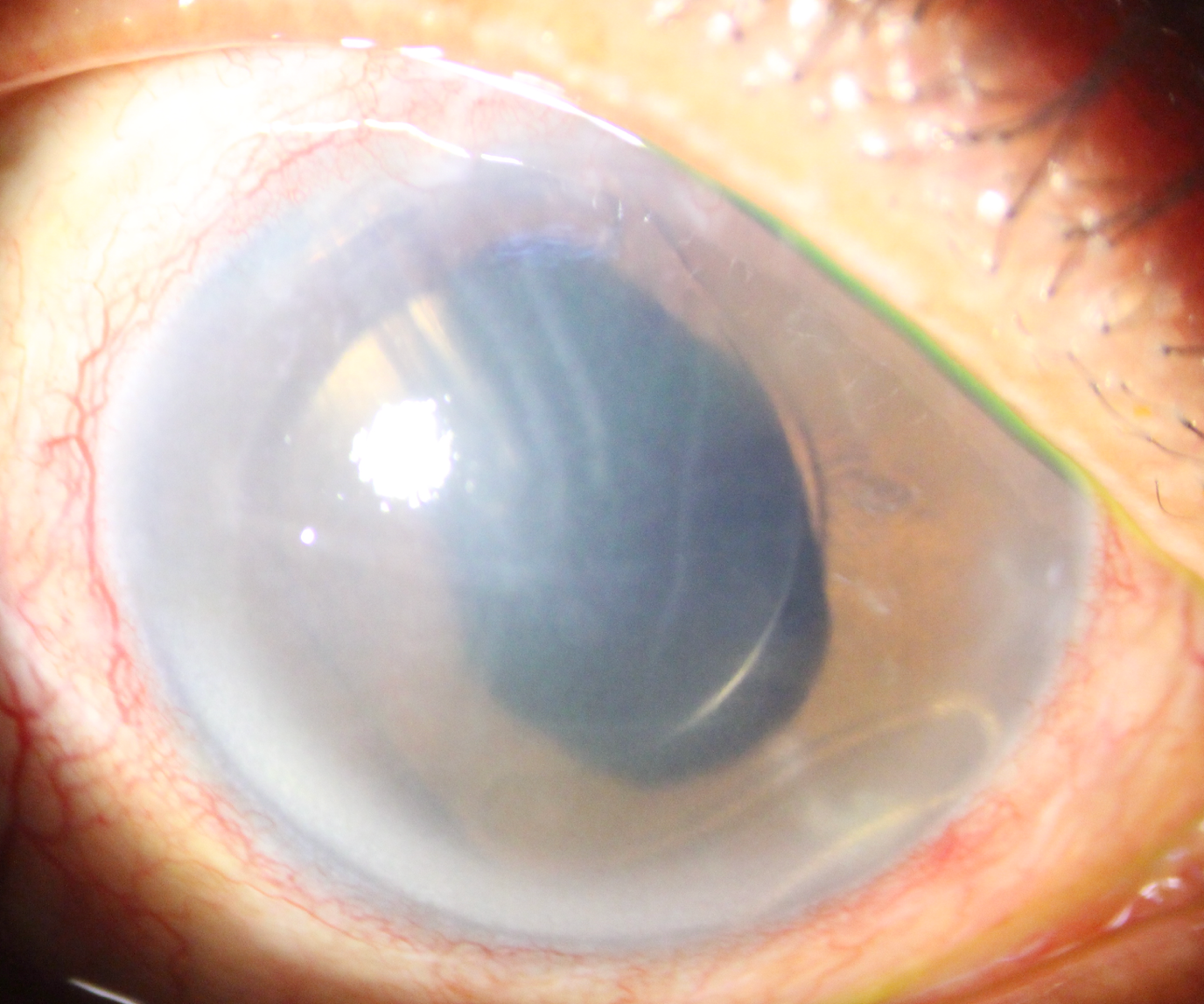
Patients usually start to notice blurred vision upon waking up because there is minimal evaporation of the tear film at night with the eyes closed, causing corneal edema. Subsequently, the blurring of vision can extend throughout the day. In patients who have undergone cataract surgery, blurry vision may persist or worsen even after months or years. As the corneal edema worsens, bullae will appear and rupture, causing severe pain, which may be accompanied by constant tearing, a foreign body sensation, redness, photophobia, and intense glare. Some patients may even notice a grayish-white discoloration of the cornea, contributing to an unsightly cosmetic blemish, especially in working or younger patients.
Management of PBK is typically approached with medical treatment first. Topical eye drops, such as hypertonic saline (sodium chloride 5%), are prescribed to create a hypertonic tear film surface, drawing fluid out of the cornea and thereby reducing corneal swelling. In the event of ruptured epithelial bullae, treatment with antibiotics and lubricating drops, along with the use of a bandage contact lens, is recommended. Sometimes, ruptured bullae can become infected and need to be treated promptly as infective keratitis.
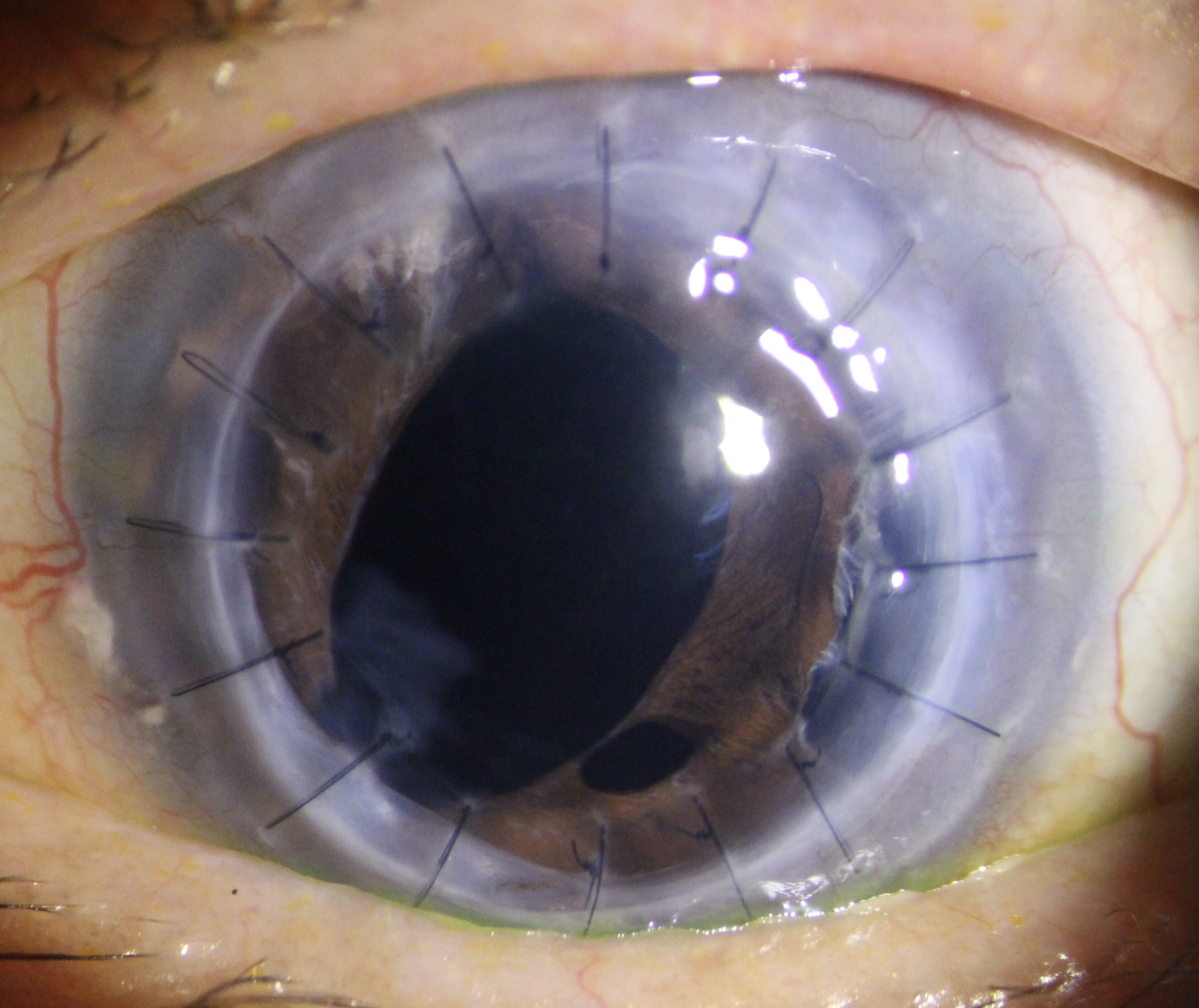
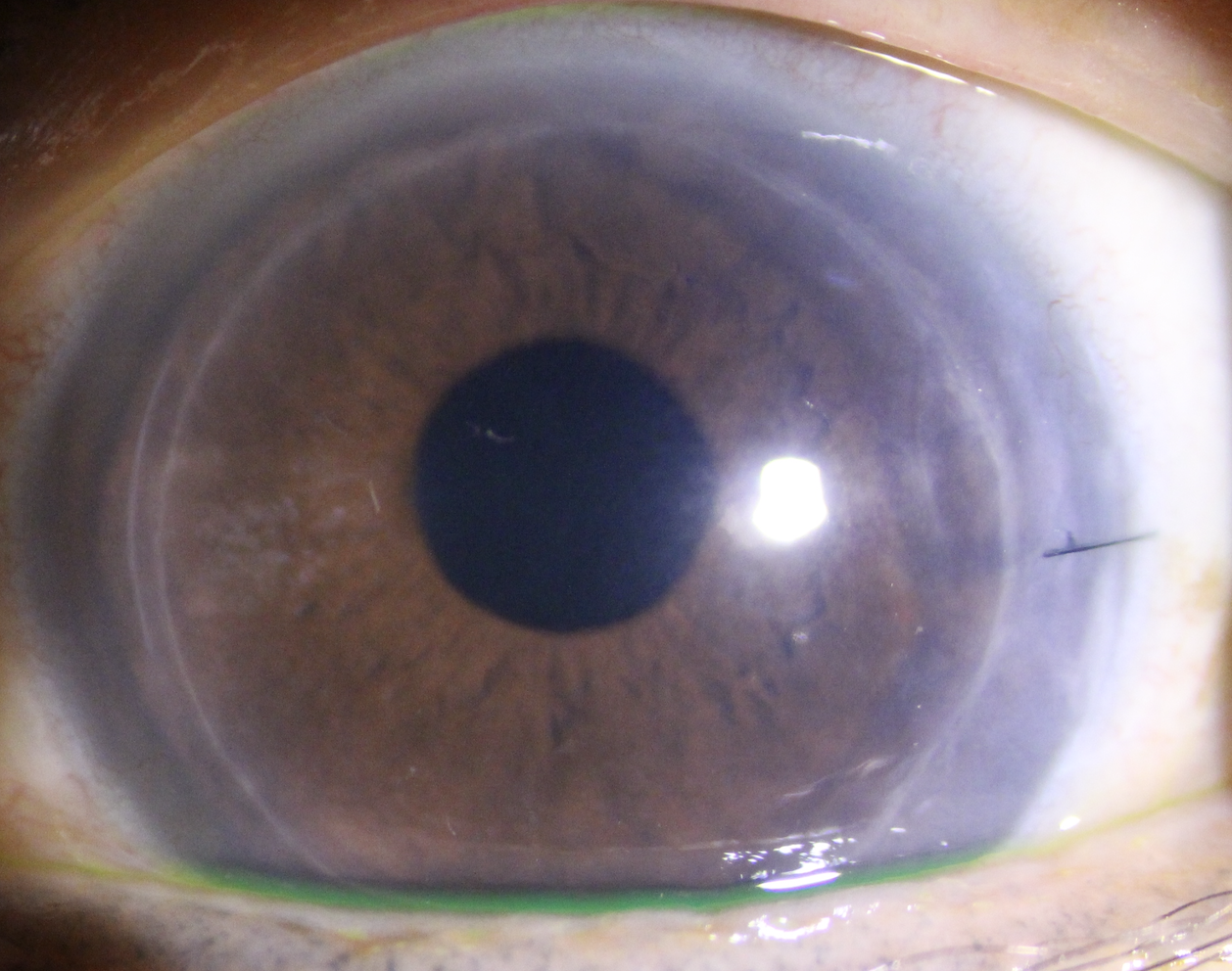
Nevertheless, corneal transplantation is the ultimate treatment for PBK as it reinstitutes the normal structure as well as the function of endothelial cells. There are few surgical methods in the form of penetrating keratoplasty (whole cornea layer), Descemet stripping automated endothelial keratoplasty (DSAEK), or Descemet membrane endothelial keratoplasty (DMEK) which both involve the posterior layer/ lamellar) only. The main goal is to replace the damaged endothelium with a healthy endothelium from a donor. Penetrating keratoplasty (PK) or a whole layer transplant (Figure 3) is indicated in cases where the bullous keratoplasty has been long-standing with cornea scarring. DSAEK (Figure 4) or DMEK has been the preferred choice for corneal transplant as the recovery is faster with a lower graft rejection rate.
Nevertheless, corneal transplantation is the ultimate treatment for PBK as it restores both the normal structure and function of endothelial cells. There are several surgical methods available: penetrating keratoplasty (PK), which involves replacing the entire corneal layer; Descemet stripping automated endothelial keratoplasty (DSAEK); and Descemet membrane endothelial keratoplasty (DMEK), both of which involve only the posterior layer or lamellar. The main goal is to replace the damaged endothelium with a healthy endothelium from a donor. Penetrating keratoplasty (PK) or a whole layer transplant (Figure 3) is indicated in cases where the bullous keratoplasty has been long-standing with cornea scarring. DSAEK (Figure 4) or DMEK has been the preferred choice for corneal transplants due to their faster recovery times and lower graft rejection rates.
Regardless of how good your eyesight is, scheduling regular eye exams is an essential way to protect overall health and wellness. Visit https://www.kpjhealth.com.my/cfs/cornea and browse through KPJ Centre For Sight social media pages: Facebook, Instagram and TikTok for more info.
This content is provided by KPJ Centre For Sight.
The views expressed here are those of the author/contributor and do not necessarily represent the views of Malaysiakini.
Interested in having your press releases, exclusive interviews, or branded content articles on Malaysiakini? For more information, contact [email protected] or [email protected].

